Wisdom teeth are a type of molar. Molars are the large chewing teeth found in the back of your mouth. Most people have three molars in each quadrant of their mouth. The last molars, or third molars, are the wisdom teeth. They’re called “wisdom teeth” because they come in late, during early adulthood, when people are “wiser” than they were as children. For most people, wisdom teeth come in between age 18 and 24. If there is not enough room in the mouth, the teeth will never fully erupt and become impacted. Impacted wisdom teeth can cause problems and often times need to be removed surgically.
Wisdom Teeth
West Hill Family Dental Wisdom Treatment

Types of Impacted Wisdom Teeth
A wisdom tooth is considered impacted when it fails to fully erupt, or emerge into its expected position. Failure to erupt may occur because of multiple reasons. First, there is not enough room in your jaw to accommodate the tooth. Second, the tooth’s eruption path is obstructed by other teeth. Finally, the angulation of the tooth is improper. These types of impactions are described by the following terms:
- Mesial Impaction – the tooth is angled forward, toward the front of the mouth. This is the most common type of impaction.
- Vertical Impaction – has a normal vertical orientation.
- Horizontal Impaction – has an alignment where the tooth is lying on its side.
- Distal Impaction – has an angulation that is generally directed towards the rear of the mouth.
In combination with the four types of impactions, wisdom teeth are also categorized as soft tissue or bony impactions.
- Partially Impacted – the upper portion of a wisdom tooth (the crown) has penetrated through the bone, but has not fully erupted through the gum tissue.
- Bony Impaction – or “fully” impacted, is when the tooth still lies mostly within the jawbone. A full-bony impaction is entirely encased by bone tissue.
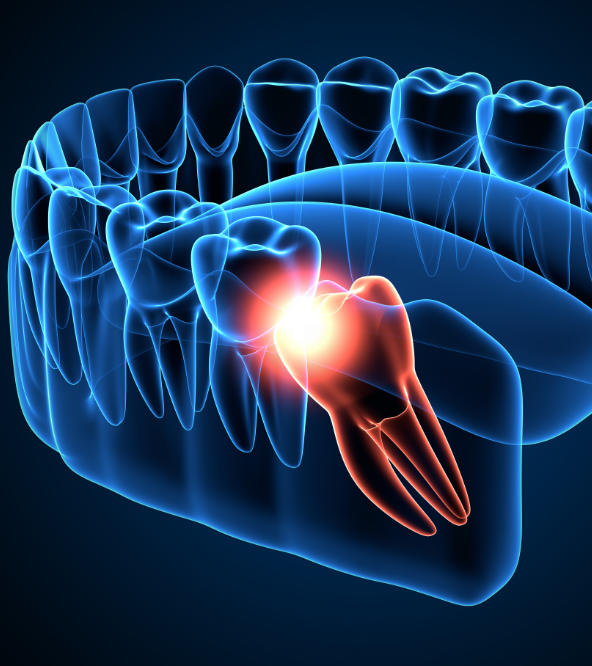
What Causes Wisdom Teeth Impaction?
The answer to this question is not always so easy. The most common answer is there is not enough jawbone space behind a person’s second molar to accommodate a third molar. What causes this lack of space is not fully understood. People with larger teeth and smaller jaws are more likely to have impacted wisdom teeth.
Am I a Good Candidate for Wisdom Teeth Removal?
There are several scenarios the make people good candidates for wisdom teeth removal:
- Pericoronitis Infection – refers to a bacterial infection in the soft tissue that surrounds the crown portion of a partially erupted tooth.
- Tooth Decay – If a partially erupted wisdom tooth has excessive decay that cannot be easily treated.
- Gum Disease Risk – When a partially erupted wisdom tooth has a portion of gum tissue that lies over the chewing surface it can be impossible to access and clean the tooth, resulting in an increase in caries risk.
- Pain – pressure from wisdom teeth pressing against your other teeth and nerves in order to find room.
- Poorly Positioned – The final position of the erupted tooth can cause problems with the cheeks when chewing.
Wisdom Teeth Removal Procedure
Before surgery, you’ll meet with the surgeon and talk about the process, expectations as well as review medical and dental history. You’ll discuss any health problems and go over any medications you’re taking. You’ll have a chance to ask any questions you have about the surgery.
During the Surgery – The surgery will usually take one hour or less. You will receive one of three types of anesthesia: Local, IV, or General. Local anesthesia includes only numbing your tooth and the surrounding tissue. It may include the use of nitrous oxide to help you relax. With IV sedation your mouth will be numbed and you’ll also receive a drug through a vein in your arm to make you drowsy. If you receive general anesthesia you will be asleep the whole time and will usually be in a hospital setting.
After the Surgery – Everyone responds differently to anesthesia. If you received local anesthesia, you’ll feel alert and might be able to drive home on your own. If you had IV or general anesthesia, you’ll need someone to drive you home. Under most circumstances, you will experience some pain and swelling post-surgery. Dr. Hemphill may decide to prescribe some pain medication if indicated. Your mouth will need a few weeks to completely heal.
Care of Mouth After Extraction:
- Do Not Rinse Mouth Day of Extraction – Rinsing your mouth should be done at least 24 hours after the extraction. Gently rinse your mouth with a glass of warm salt water (1/4 teaspoon salt per glass of water). Rinse gently after meals and multiple times per day.
- Bleeding – Following extractions some bleeding is to be expected. If persistent bleeding occurs, place gauze pads over the bleeding area and bite down firmly for 30 minutes. Repeat if necessary.
- Swelling – Some swelling is not uncommon. Ice bag or chopped ice wrapped in a towel should be applied to the operated area for 30 minutes every 4 hours as needed.
- Pain – most of the time there will be some discomfort. non-aspirin types of medications will be best if there are no medical contraindications. Ask Dr. Hemphill what pain medication will be best for you.
- Food – soft, cool, mushy foods will be best for the first couple of days. Avoid hot foods and liquids as these will encourage bleeding from the extraction site. Avoid foods with tiny seeds that might get up inside the socket. Avoid using a straw when drinking.
- Smoking – No smoking allowed after the first 48 hours. Smoking may cause the clot to bleed as well as cause inefficient healing.
- Bony edges – small bone fragments are common and my show up around the extraction site at any time. These are not roots of the tooth. If they bother you, please make an appointment to return to have Dr. Hemphill remove them from your tissue.